
Home » The Pulse on Study Conduct
The Pulse on Study Conduct
January 8, 2018
Educate yourself on new therapeutic areas
Medical knowledge for the vast assimilation of clinical research guidelines is necessary for anyone entering the field. The diverse regulatory landscape requires us to stay abreast of changes that impact patient safety data. It is a multifaceted learning process with educational requirements that vary by role. We should never expect anyone to have every answer, or to know everything about a protocol/therapeutic area. That sets an unrealistic standard that undermines performance.
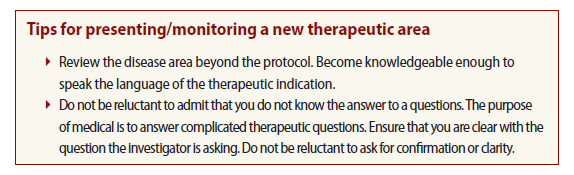
Whenever assigned to a new study therapeutic area, I prepare enough to effectively discuss the trial design, study drug and eligibility criteria with investigational staff during site assessment. I want to provide critical details beyond the protocol so that they can make an informed decision regarding their capabilities for study participation. The extent to which I learn the therapeutic area is more than what is expected for a preliminary study discussion, but this ensures sponsor and site satisfaction.
Many years ago, I was assigned to select sites for a rare disease study. The first investigators with whom I was scheduled to meet were therapeutic experts; M.D./Ph.D.s who had advised on trial design, compound development or both. It was a brand new clinical area for me, and while eager to learn, I also felt trepidation over presenting to clinical experts as a novice. The study project manager repeatedly informed me that every investigator and site visit was high-profile. However, nothing was as important as the first study meeting at the site scheduled for first patient screened. This critical milestone hinged on this site, and the magnitude portrayed by the study manager’s email instruction for the meeting read like the declaration of independence to colonial Americans. “Exceptionally important site to the sponsor!” “Focus only on high-level information due to expertise!” “Confirm eligibility potential of first patient screened!” “Gently encourage the site to provide the first screening date!”
In other words, I was to present the protocol to the M.D. scientist who had helped design it, confirm their patient met eligibility criteria, and gently urge them to rapid screening in an area where they were international experts and I was the beginner, when they had a direct line to the sponsor and I communicated through an overwhelmed study manager.
Without realizing it, I was allowing the study manager’s panic to influence my impression of these investigators, to create worry where good judgement usually prevailed, and to rethink an organized process. This changed my usual process in that I found myself up to the late hours Googling every diagnostic term, re-reviewing the protocol and attempting to memorize inclusion/exclusion criteria. And for what? To serve a preconceived impression of an investigator that was formed under duress and may or may not be correct?
My good sense convinced me to shut down my computer and trust that I had prepared to the best of my ability. I could only control my reaction to the unknown and my professionalism should I be given a lukewarm reception.
The next morning, I arrived at the imposing university hospital ahead of schedule. I waited in the lobby until the study coordinator appeared to escort me back to the conference room. An individual I presumed to be the principal investigator was sitting at the conference table reading email on his phone. Before I could do so he extended his hand warmly and introduced himself as the study co-investigator. I recognized his name from the protocol as he had been quoted several times in the footnotes. He was a specialist in the indication but treated the patients in clinical practice more frequently than the principal investigator, who spent more time behind the podium speaking/lecturing or under the microscope studying new treatment.
He then proceeded to shatter any preconceived notions with his wit and we formed an instant rapport.
Several minutes later the principal investigator arrived and apologized for being late. I introduced myself, and he smiled and graciously thanked me for coming to their site. As I flipped to the start of the protocol slide deck, I informed the investigator that I was going to cover only high-level information due to his expertise. The Principal Investigator’s response surprised me more than his colleagues had. He asked me to please cover everything that was required to adequately conduct the visit. He offered to supplement the protocol information with specific data from the earlier trials, if I was interested.
After I reviewed the study information I asked the investigator about his plan for identifying patients. The indication was rare and the enrollment process was expected to be laborious due to this. The investigator provided a comprehensive plan for patient identification that included genetic databases and area colleague referral. He had clearly deliberated the process with his team, which accounted for his transparency, as opposed to rote proclamations of enrollment prowess based on expertise.
The meeting was extremely positive. Both investigators were appreciative of the information I provided and happily answered all my questions. They were self-effacing, funny, and gracious. An important lesson beyond the new therapeutic area was learned by me that day. Judge the package by the content and not the cover.
Elizabeth Blair Weeks-Rowe, LVN, CCRA, has spent nearly 14 years in a variety of clinical research roles including CRA, CRA trainer, CRA manager and clinical research writer. Email ebwcra@yahoo.com or tweet @ebwcra.




